| Aspergillosis | |
|---|---|
 | |
| Tomosynthesis of chronic fibrosing pulmonary aspergillosis | |
| Pronunciation |
|
| Specialty | Infectious disease |
| Complications | Bleeding, Systemic infection.[1] |
| Frequency | 14 million |
Aspergillosis is a fungal infection of usually the lungs,[2] caused by the genus Aspergillus, a common mould that is breathed in frequently from the air, but does not usually affect most people.[3][4] It generally occurs in people with lung diseases such as asthma, cystic fibrosis or tuberculosis, or those who are immunocompromized such as those who have had a stem cell or organ transplant or those who take medications such as steroids and some cancer treatments which suppress the immune system.[2][5] Rarely, it can affect skin.[5][6]
Aspergillosis occurs in humans, birds and other animals. Aspergillosis occurs in chronic or acute forms which are clinically very distinct. Most cases of acute aspergillosis occur in people with severely compromised immune systems such as those undergoing bone marrow transplantation.[7] Chronic colonization or infection can cause complications in people with underlying respiratory illnesses, such as asthma,[8] cystic fibrosis,[9] sarcoidosis,[10] tuberculosis, or chronic obstructive pulmonary disease.[11] Most commonly, aspergillosis occurs in the form of chronic pulmonary aspergillosis (CPA), aspergilloma, or allergic bronchopulmonary aspergillosis (ABPA).[12] Some forms are intertwined; for example ABPA and simple aspergilloma can progress to CPA.
Other, noninvasive manifestations include fungal sinusitis (both allergic in nature and with established fungal balls), otomycosis (ear infection), keratitis (eye infection), and onychomycosis (nail infection). In most instances, these are less severe, and curable with effective antifungal treatment.
The most frequently identified pathogens are Aspergillus fumigatus and Aspergillus flavus, ubiquitous organisms capable of living under extensive environmental stress. Most people are thought to inhale thousands of Aspergillus spores daily but without effect due to an efficient immune response. Invasive aspergillosis has a 20% mortality at 6 months.[13] The major chronic, invasive, and allergic forms of aspergillosis account for around 600,000 deaths annually worldwide.[10][14][15][16][17]
Signs and symptoms
A fungus ball in the lungs may cause no symptoms and may be discovered only with a chest X-ray, or it may cause repeated coughing up of blood, chest pain, and occasionally severe, even fatal, bleeding.[2] A rapidly invasive Aspergillus infection in the lungs often causes cough, fever, chest pain, and difficulty breathing.
Poorly controlled aspergillosis can disseminate through the blood to cause widespread organ damage.[2] Symptoms include fever, chills, shock, delirium, seizures, and blood clots. The person may develop kidney failure, liver failure (causing jaundice), and breathing difficulties.[2] Death can occur quickly.
Aspergillosis of the ear canal causes itching and occasionally pain. Fluid draining overnight from the ear may leave a stain on the pillow. Aspergillosis of the sinuses causes a feeling of congestion and sometimes pain or discharge. It can extend beyond the sinuses.[18]
Cause

Aspergillosis is caused by Aspergillus, a common mold, which tends to affect people who already have a lung disease such as cystic fibrosis or asthma, or who cannot fight infection themselves.[3] The most common causative species is Aspergillus fumigatus.[19]
Risk factors
People who are immunocompromised — such as patients undergoing hematopoietic stem cell transplantation, chemotherapy for leukaemia, or AIDS — are at an increased risk for invasive aspergillosis infections. These people may have neutropenia or corticosteroid-induced immunosuppression as a result of medical treatments. Neutropenia is often caused by extremely cytotoxic medications such as cyclophosphamide. Cyclophosphamide interferes with cellular replication including that of white blood cells such as neutrophils. A decreased neutrophil count inhibits the ability of the body to mount immune responses against pathogens. Although tumor necrosis factor alpha (TNF-α) — a signaling molecule related to acute inflammation responses — is produced, the abnormally low number of neutrophils present in neutropenic patients leads to a depressed inflammatory response. If the underlying neutropenia is not fixed, rapid and uncontrolled hyphal growth of the invasive fungi will occur and result in negative health outcomes.[20] In addition to decreased neutrophil degranulation, the antiviral response against Flu and SARS-CoV-2 viruses, mediated by type I and type II interferon, is diminished jointly with the local antifungal immune response measured in the lungs of patients with IAPA (Influenza-Associated Pulmonary Aspergillosis) and CAPA (COVID-19-Associated Pulmonary Aspergillosis).[21] COVID-19 patients with preexisting or newly diagnosed bronchiectasis are at particular risk of developing pulmonary aspergillosis.[22]
Normally the mucociliary clearance mechanism of the airways of the lungs removes inhaled particles. However, in those with underlying lung diseases, such as cystic fibrosis or bronchiectasis, this mucociliary clearance mechanism is impaired and aspergillus spores (which are 2-5 μm in diameter) are able to colonize the airways and sinuses.[13]
Diagnosis

On chest X-ray and CT, pulmonary aspergillosis classically manifests as a halo sign, and later, an air crescent sign.[24] In hematologic patients with invasive aspergillosis, the galactomannan test can make the diagnosis in a noninvasive way. Galactomannan is a component of the fungal wall.[13] False-positive Aspergillus galactomannan tests have been found in patients on intravenous treatment with some antibiotics or fluids containing gluconate or citric acid such as some transfusion platelets, parenteral nutrition, or PlasmaLyte.[25][26]
On microscopy, Aspergillus species are reliably demonstrated by silver stains, e.g., Gridley stain or Gomori methenamine-silver.[27] These give the fungal walls a gray-black colour. The hyphae of Aspergillus species range in diameter from 2.5 to 4.5 μm. They have septate hyphae,[28] but these are not always apparent, and in such cases they may be mistaken for Zygomycota.[27] Aspergillus hyphae tend to have dichotomous branching that is progressive and primarily at acute angles of around 45°.[27]
In those with suspected pulmonary aspergillosis, bronchoalveolar lavage can be done to collect fluid from the airways of the lungs for analysis. This involves exploration of the airway with a bronchoscope, then the introduction of a small amount of fluid into the airway which is then collected for analysis. This analysis can include assessment of cells, galactomannan testing, staining and fungal culture as well as polymerase chain reaction (PCR) assessment.[13] PCR has an 85% sensitivity and 76% specificity for the diagnosis of aspergillosis, sensitivity is increased when the test is combined with galactomannan testing.[13]
Allergic bronchopulmonary aspergillosis (ABPA) is diagnosed by establishing an immune sensitization to aspergillosis, which can be done by measuring total eosinophils, total immunoglobulin E (IgE) and aspergillus specific IgE and IgG levels. Elevations of these markers, combined with clinical and radiologic findings suggesting infection are used to confirm ABPA.[13]
_invasive_type.jpg.webp) Pulmonary invasive aspergillosis in a person with interstitial pneumonia (autopsy material), using Grocott's methenamine silver stain
Pulmonary invasive aspergillosis in a person with interstitial pneumonia (autopsy material), using Grocott's methenamine silver stain Angioinvasive pulmonary aspergillosis
Angioinvasive pulmonary aspergillosis_invasive_type.jpg.webp) Angioinvasive pulmonary aspergillosis (closeup)
Angioinvasive pulmonary aspergillosis (closeup)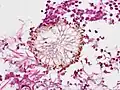 Aspergillus vesicle (HE stain)
Aspergillus vesicle (HE stain)
Prevention
Prevention of aspergillosis involves a reduction of mold exposure via environmental infection-control. Antifungal prophylaxis can be given to high-risk patients. Posaconazole is often given as prophylaxis in severely immunocompromised patients.[29]
Screening
A systematic review has evaluated the diagnostic accuracy of polymerase chain reaction (PCR) tests in people with defective immune systems from medical treatment such as chemotherapy.[30] Evidence suggests PCR tests have moderate diagnostic accuracy when used for screening for invasive aspergillosis in high risk groups.[30] CT and MRI are vital to diagnosis, however it is always highly recommended to under go a biopsy of the area to confirm a diagnosis.[31][32][33]
Treatment
The current medical treatments for aggressive invasive aspergillosis include voriconazole and liposomal amphotericin B in combination with surgical debridement.[34] For the less aggressive allergic bronchopulmonary aspergillosis, findings suggest the use of oral steroids for a prolonged period of time, preferably for 6–9 months in allergic aspergillosis of the lungs. Itraconazole is given with the steroids, as it is considered to have a "steroid-sparing" effect, causing the steroids to be more effective, allowing a lower dose.[35] Other drugs used, such as amphotericin B, caspofungin (in combination therapy only), flucytosine (in combination therapy only), or itraconazole,[36][37] are used to treat this fungal infection. However, a growing proportion of infections are resistant to the triazoles.[38] A. fumigatus, the most commonly infecting species, is intrinsically resistant to fluconazole.[39]
Epidemiology
Aspergillosis is thought to affect more than 14 million people worldwide, with allergic bronchopulmonary aspergillosis (ABPA) infecting about 4 million, severe asthma with fungal sensitization affecting about 6.5 million, and chronic pulmonary aspergillosis infecting about 3 million people, considerably more than invasive aspergillosis which affects about 300,000 people.[40] Other common conditions include Aspergillus bronchitis, Aspergillus rhinosinusitis, or otitis externa.[41][42]
Society and culture
During the COVID-19 pandemic 2020/21, COVID-19-associated pulmonary aspergillosis was reported in some people who had been admitted to hospital and received longterm steroid treatment.[43]
Animals
While relatively rare in humans, aspergillosis is a common and dangerous infection in birds, particularly in pet parrots. Mallards and other ducks are particularly susceptible, as they often resort to poor food sources during bad weather. Captive raptors, such as falcons and hawks, are susceptible to this disease if they are kept in poor conditions and especially if they are fed pigeons, which are often carriers of "asper". It can be acute in chicks, but chronic in mature birds.
In the United States, aspergillosis has been the culprit in several rapid die-offs among waterfowl. From 8 December until 14 December 2006, over 2,000 mallards died near Burley, Idaho, an agricultural community about 150 miles southeast of Boise. Mouldy waste grain from the farmland and feedlots in the area is the suspected source. A similar aspergillosis outbreak caused by mouldy grain killed 500 mallards in Iowa in 2005.
While no connection has been found between aspergillosis and the H5N1 strain of avian influenza (commonly called "bird flu"), rapid die-offs caused by aspergillosis can spark fears of bird flu outbreaks. Laboratory analysis is the only way to distinguish bird flu from aspergillosis.
In dogs, aspergillosis is an uncommon disease typically affecting only the nasal passages (nasal aspergillosis). This is much more common in dolicocephalic breeds. It can also spread to the rest of the body; this is termed disseminated aspergillosis and is rare, usually affecting individuals with underlying immune disorders.
In 2019, an outbreak of aspergillosis struck the rare kākāpō, a large flightless parrot endemic to New Zealand. By June the disease had killed seven of the birds, whose total population at the time was only 142 adults and 72 chicks. One fifth of the population was infected with the disease and the entire species was considered at risk of extinction.[44]
See also
- Other ways in which aspergillus can cause disease in mammals:
References
- ↑ "Aspergillosis". mayoclinic.org. Mayo Clinic. Retrieved June 5, 2022.
- 1 2 3 4 5 Thornton CR (2020). "1. Detection of the 'Big Five' mold killers of humans: Aspergillus, Fusarium, Lomentospora, Scedosporium and Mucormycetes". In Gadd GM, Sariaslani S (eds.). Advances in Applied Microbiology. Academic Press. pp. 4–22. ISBN 978-0-12-820703-1.
- 1 2 "ICD-11 - ICD-11 for Mortality and Morbidity Statistics". World Health Organization. Retrieved 29 May 2021.
- ↑ "Aspergillosis | About". www.cdc.gov. 10 May 2021. Retrieved 1 June 2021.
- 1 2 Kutzner H, Kempf W, Feit J, Sangueza O (2021). "2. Fungal infections". Atlas of Clinical Dermatopathology: Infectious and Parasitic Dermatoses. Hoboken: Wiley Blackwell. p. 103-104. ISBN 978-1-119-64706-5.
- ↑ Johnstone RB (2017). "25. Mycoses and Algal infections". Weedon's Skin Pathology Essentials (2nd ed.). Elsevier. p. 463. ISBN 978-0-7020-6830-0.
- ↑ "Invasive pulmonary aspergillosis | Aspergillus & Aspergillosis Website". The Aspergillus Website. Archived from the original on 26 July 2020. Retrieved 28 June 2019.
- ↑ Denning DW, Pashley C, Hartl D, Wardlaw A, Godet C, Del Giacco S, et al. (15 April 2014). "Fungal allergy in asthma-state of the art and research needs". Clinical and Translational Allergy. 4 (1): 14. doi:10.1186/2045-7022-4-14. PMC 4005466. PMID 24735832.
- ↑ Warris A, Bercusson A, Armstrong-James D (April 2019). "Aspergillus colonization and antifungal immunity in cystic fibrosis patients". Medical Mycology. 57 (Supplement_2): S118–S126. doi:10.1093/mmy/myy074. hdl:2164/13751. PMID 30816976.
- 1 2 Denning DW, Pleuvry A, Cole DC (March 2013). "Global burden of chronic pulmonary aspergillosis complicating sarcoidosis". The European Respiratory Journal. 41 (3): 621–626. doi:10.1183/09031936.00226911. PMID 22743676. S2CID 8823691.
- ↑ Smith NL, Denning DW (April 2011). "Underlying conditions in chronic pulmonary aspergillosis including simple aspergilloma". The European Respiratory Journal. 37 (4): 865–872. doi:10.1183/09031936.00054810. PMID 20595150. S2CID 18292691.
- ↑ Goel A. "Pulmonary aspergillosis". Mediconotebook. Retrieved 29 May 2015.
- 1 2 3 4 5 6 Thompson, George R.; Young, Jo-Anne H. (14 October 2021). "Aspergillus Infections". New England Journal of Medicine. 385 (16): 1496–1509. doi:10.1056/NEJMra2027424.
- ↑ Guinea J, Torres-Narbona M, Gijón P, Muñoz P, Pozo F, Peláez T, et al. (July 2010). "Pulmonary aspergillosis in patients with chronic obstructive pulmonary disease: incidence, risk factors, and outcome". Clinical Microbiology and Infection. 16 (7): 870–877. doi:10.1111/j.1469-0691.2009.03015.x. PMID 19906275.
- ↑ Chen J, Yang Q, Huang J, Li L (September 2013). "Risk factors for invasive pulmonary aspergillosis and hospital mortality in acute-on-chronic liver failure patients: a retrospective-cohort study". International Journal of Medical Sciences. 10 (12): 1625–1631. doi:10.7150/ijms.6824. PMC 3804788. PMID 24151434.
- ↑ Garcia-Vidal C, Upton A, Kirby KA, Marr KA (October 2008). "Epidemiology of invasive mold infections in allogeneic stem cell transplant recipients: biological risk factors for infection according to time after transplantation". Clinical Infectious Diseases. 47 (8): 1041–1050. doi:10.1086/591969. PMC 2668264. PMID 18781877.
- ↑ Nam HS, Jeon K, Um SW, Suh GY, Chung MP, Kim H, et al. (June 2010). "Clinical characteristics and treatment outcomes of chronic necrotizing pulmonary aspergillosis: a review of 43 cases". International Journal of Infectious Diseases. 14 (6): e479–e482. doi:10.1016/j.ijid.2009.07.011. PMID 19910234.
- ↑ Ederies A, Chen J, Aviv RI, Pirouzmand F, Bilbao JM, Thompson AL, Symons SP (May 2010). "Aspergillosis of the Petrous Apex and Meckel's Cave". Skull Base. 20 (3): 189–192. doi:10.1055/s-0029-1246229. PMC 3037105. PMID 21318037.
- ↑ Willinger G (2019). "1. What is the target? Clinical mycology and diagnostics". In Presterl E (ed.). Clinically Relevant Mycoses: A Practical Approach. Springer. pp. 3–19. ISBN 978-3-319-92299-7.
- ↑ Dagenais TR, Keller NP (July 2009). "Pathogenesis of Aspergillus fumigatus in Invasive Aspergillosis". Clinical Microbiology Reviews. 22 (3): 447–465. doi:10.1128/CMR.00055-08. PMC 2708386. PMID 19597008.
- ↑ Feys S, Gonçalves SM, Khan M, Choi S, Boeckx B, Chatelain D, et al. (August 2022). "Lung epithelial and myeloid innate immunity in influenza-associated or COVID-19-associated pulmonary aspergillosis: an observational study". The Lancet Respiratory Medicine. 10 (12): 1147–1159. doi:10.1016/S2213-2600(22)00259-4. PMC 9401975. PMID 36029799.
- ↑ Baratella, Elisa; Roman-Pognuz, Erik; Zerbato, Verena; Minelli, Pierluca; Cavallaro, Marco Francesco Maria; Cova, Maria Assunta; Luzzati, Roberto; Lucangelo, Umberto; Sanson, Gianfranco; Friso, Federica; Bussani, Rossana; Pinamonti, Maurizio; Busetti, Marina; Salton, Francesco; Confalonieri, Marco (2021-12-30). "Potential links between COVID-19-associated pulmonary aspergillosis and bronchiectasis as detected by high resolution computed tomography". Frontiers in Bioscience-Landmark. 26 (12): 1607–1612. doi:10.52586/5053. hdl:11368/3004919. ISSN 2768-6701.
- ↑ Snoeckx A, Reyntiens P, Desbuquoit D, Spinhoven MJ, Van Schil PE, van Meerbeeck JP, Parizel PM (February 2018). "Evaluation of the solitary pulmonary nodule: size matters, but do not ignore the power of morphology". Insights into Imaging. 9 (1): 73–86. doi:10.1007/s13244-017-0581-2. PMC 5825309. PMID 29143191.
- ↑ Curtis AM, Smith GJ, Ravin CE (October 1979). "Air crescent sign of invasive aspergillosis". Radiology. 133 (1): 17–21. doi:10.1148/133.1.17. PMID 472287.
- ↑ Fortún J, Martín-Dávila P, Alvarez ME, Norman F, Sánchez-Sousa A, Gajate L, et al. (January 2009). "False-positive results of Aspergillus galactomannan antigenemia in liver transplant recipients". Transplantation. 87 (2): 256–260. doi:10.1097/TP.0b013e31819288d5. PMID 19155981. S2CID 40438193.
- ↑ Martín-Rabadán P, Gijón P, Alonso Fernández R, Ballesteros M, Anguita J, Bouza E (August 2012). "False-positive Aspergillus antigenemia due to blood product conditioning fluids". Clinical Infectious Diseases. 55 (4): e22–e27. doi:10.1093/cid/cis493. PMID 22610929.
- 1 2 3 Kradin RL, Mark EJ (April 2008). "The pathology of pulmonary disorders due to Aspergillus spp". Archives of Pathology & Laboratory Medicine. 132 (4): 606–614. doi:10.5858/2008-132-606-TPOPDD. PMID 18384212.
- ↑ "Mycoses: Aspergillosis". Mycology Online. Archived from the original on 7 December 2008. Retrieved 2008-12-10.
- ↑ Cornely OA, Maertens J, Winston DJ, Perfect J, Ullmann AJ, Walsh TJ, et al. (January 2007). "Posaconazole vs. fluconazole or itraconazole prophylaxis in patients with neutropenia". The New England Journal of Medicine. 356 (4): 348–359. doi:10.1056/NEJMoa061094. PMID 17251531. S2CID 40335480.
- 1 2 Cruciani M, Mengoli C, Barnes R, Donnelly JP, Loeffler J, Jones BL, et al. (September 2019). "Polymerase chain reaction blood tests for the diagnosis of invasive aspergillosis in immunocompromised people". The Cochrane Database of Systematic Reviews. 2019 (9): CD009551. doi:10.1002/14651858.cd009551.pub4. PMC 6719256. PMID 31478559.
- ↑ Harris GJ, Will BR (1989). "Orbital aspergillosis. Conservative debridement and local amphotericin irrigation". Ophthalmic Plastic and Reconstructive Surgery. 5 (3): 207–211. doi:10.1097/00002341-198909000-00012. PMID 2487225.
- ↑ Kopp W, Fotter R, Steiner H, Beaufort F, Stammberger H (September 1985). "Aspergillosis of the paranasal sinuses". Radiology. 156 (3): 715–716. doi:10.1148/radiology.156.3.4023231. PMID 4023231.
- ↑ Hutnik CM, Nicolle DA, Munoz DG (December 1997). "Orbital aspergillosis. A fatal masquerader". Journal of Neuro-Ophthalmology. 17 (4): 257–261. doi:10.1097/00041327-199712000-00009. PMID 9427179.
- ↑ Kontoyiannis DP, Lionakis MS, Lewis RE, Chamilos G, Healy M, Perego C, et al. (April 2005). "Zygomycosis in a tertiary-care cancer center in the era of Aspergillus-active antifungal therapy: a case-control observational study of 27 recent cases". The Journal of Infectious Diseases. 191 (8): 1350–1360. doi:10.1086/428780. PMID 15776383.
- ↑ Walsh TJ, Anaissie EJ, Denning DW, Herbrecht R, Kontoyiannis DP, Marr KA, et al. (February 2008). "Treatment of aspergillosis: clinical practice guidelines of the Infectious Diseases Society of America". Clinical Infectious Diseases. 46 (3): 327–360. doi:10.1086/525258. PMID 18177225.
- ↑ Herbrecht R, Denning DW, Patterson TF, Bennett JE, Greene RE, Oestmann JW, et al. (August 2002). Invasive Fungal Infections Group of the European Organisation for Research and Treatment of Cancer and the Global Aspergillus Study Group. "Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis". The New England Journal of Medicine. 347 (6): 408–415. doi:10.1056/NEJMoa020191. hdl:2066/185528. PMID 12167683.
- ↑ Cornely OA, Maertens J, Bresnik M, Ebrahimi R, Ullmann AJ, Bouza E, et al. (May 2007). "Liposomal amphotericin B as initial therapy for invasive mold infection: a randomized trial comparing a high-loading dose regimen with standard dosing (AmBiLoad trial)". Clinical Infectious Diseases. 44 (10): 1289–1297. doi:10.1086/514341. PMID 17443465.
- ↑ Denning DW, Park S, Lass-Florl C, Fraczek MG, Kirwan M, Gore R, et al. (May 2011). "High-frequency triazole resistance found In nonculturable Aspergillus fumigatus from lungs of patients with chronic fungal disease". Clinical Infectious Diseases. 52 (9): 1123–1129. doi:10.1093/cid/cir179. PMC 3106268. PMID 21467016.
- ↑ Perea S, Patterson TF (November 2002). "Antifungal resistance in pathogenic fungi". Clinical Infectious Diseases. 35 (9): 1073–1080. doi:10.1086/344058. PMID 12384841.
- ↑ Bongomin F, Gago S, Oladele RO, Denning DW (October 2017). "Global and Multi-National Prevalence of Fungal Diseases-Estimate Precision". Journal of Fungi. 3 (4): 57. doi:10.3390/jof3040057. PMC 5753159. PMID 29371573.
- ↑ Bongomin F, Batac CR, Richardson MD, Denning DW (June 2018). "A Review of Onychomycosis Due to Aspergillus Species". Mycopathologia. 183 (3): 485–493. doi:10.1007/s11046-017-0222-9. PMC 5958150. PMID 29147866.
- ↑ "Aspergillus bronchitis | Aspergillus & Aspergillosis Website". www.aspergillus.org.uk.
- ↑ Machado M, Valerio M, Álvarez-Uría A, Olmedo M, Veintimilla C, Padilla B, et al. (February 2021). "Invasive pulmonary aspergillosis in the COVID-19 era: An expected new entity". Mycoses. 64 (2): 132–143. doi:10.1111/myc.13213. PMC 7753705. PMID 33210776.
- ↑ Anderson C (2019-06-13). "World's fattest parrot, the endangered kākāpō, could be wiped out by fungal infection". The Guardian. ISSN 0261-3077. Retrieved 2019-06-13.