| Diverticulum | |
|---|---|
| Other names | Diverticula |
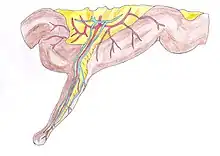
 | |
| Schematic drawing of a false diverticulum. A - mucosa; B - submucosa; C - muscularis; D - serosa and subserosa | |
| Specialty | Gastroenterology |
In medicine or biology, a diverticulum is an outpouching of a hollow (or a fluid-filled) structure in the body.[1] Depending upon which layers of the structure are involved, diverticula are described as being either true or false.[2]
In medicine, the term usually implies the structure is not normally present, but in embryology, the term is used for some normal structures arising from others, as for instance the thyroid diverticulum, which arises from the tongue.[3]
The word comes from Latin dīverticulum, "bypath" or "byway".
Classification
Diverticula are described as being true or false depending upon the layers involved:
- False diverticula (also known as "pseudodiverticula") do not involve muscular layers or adventitia. False diverticula, in the gastrointestinal tract for instance, involve only the submucosa and mucosa, such as Zenker's diverticulum.[2] False diverticula are typically synonymous with pulsion diverticula, which describes the mechanism of formation as increased intraluminal pressure.
- True diverticula involve all layers of the structure, including muscularis propria and adventitia, such as Meckel's diverticulum.[2] True diverticula are typically synonymous with traction diverticula, which describes the mechanism of formation as pulling forces external to the structure.
Embryology
- The kidneys are originally diverticula in the development of the urinary and reproductive organs.
- The lungs are originally diverticula forming off of the ventral foregut.[3]
- The thymus appears in the form of two flask-shape diverticula, which arise from the third branchial pouch (pharyngeal pouch) of the endoderm.[4]
- The thyroid gland develops as a diverticulum arising from a point on the tongue, demarcated as the foramen cecum.[3]

Human pathology
Gastrointestinal tract diverticula
- Esophageal diverticula may occur in one of three areas of the esophagus:
- Pharyngeal (Zenker's) diverticula usually occur in the elderly, through Killian's triangle between the thyropharyngeus and cricopharyngeus muscle of the inferior pharyngeal constrictors.
- Midesophageal diverticula
- Epiphrenic diverticula are due to dysfunction of the lower esophageal sphincter, as in achalasia.[5]
- A duodenal diverticulum can be found incidentally in 23% of normal people undergoing imaging. It can be either congenital or acquired, but the acquired form is more common and is due to the weakness of the duodenal wall, which causes protrusions. It is usually found at the second or third part of duodenum, around the ampulla of Vater. Food debris may enter the diverticular outpouchings, causing inflammation or diverticulitis. On CT or MRI imaging, it appears as a sac-like outpouching. If the diverticulum is filled with contrast agents, the wall would be thin and may contain air, fluid, contrast material, or food debris. If the food debris is broken down by bacteria, the outpouching may show "faeces sign". Inflammation of the duodenal wall shows thickening of the wall. Rarely, on barium studies in congenital duodenal diverticula, the contrast material fills up the true lumen, causing "windsock" deformity.[6]
- A jejunal diverticulum is a congenital lesion and may be a source of bacterial overgrowth. It may also perforate or result in abscesses.
- A Killian-Jamieson diverticulum is very similar to a pharyngeal esophageal diverticulum, differing in the fact that the pouching is between the oblique and transverse fibers of the cricopharyngeus muscle.[7]
- A Laimer diverticulum is an outpouching that occurs in the Laimer triangle between the cricopharyngeus and superior esophageal circular muscle.
- Colonic diverticula, although found incidentally during colonoscopy, may become infected (see diverticulitis) and can perforate, requiring surgery.[8]
- Gastric diverticula are very infrequent.[9]
- Meckel's diverticulum, a persistent portion of the omphalomesenteric duct, is present in 2% of the population,[10] making it the most common congenital gastrointestinal malformation.[11]

- Rokitansky-Aschoff sinuses are diverticula in the gallbladder due to chronic cholecystitis[12]
Most of these pathological types of diverticula are capable of harboring an enterolith. If the enterolith stays in place, it may cause no problems, but a large enterolith expelled from a diverticulum into the lumen can cause obstruction.[13]
Genito-urinary tract diverticula
- Bladder diverticula are balloon-like growths on the bladder commonly associated with chronic outflow obstruction, such as benign prostatic hyperplasia in older males. Usually found in pairs on opposite sides of the bladder, bladder diverticula are often surgically removed to prevent infection, rupture, or even cancer.
- Calyceal diverticula are usually asymptomatic, but if a stone becomes lodged in the outpouching, they may present with pain.[14]
- Urethral diverticula are usually found in women aged 30 to 70 years old, in between 1 and 6% of adult women. Since most cases are without any symptoms, the true incidence is unknown. Symptoms may vary from frequent urinary tract infections, painful sexual intercourse (dyspareunia), or symptoms due to cancer. A urethral diverticulum is located on the anterior vaginal wall, 1 to 3 cm inside the vaginal introitus. MRI is preferred as the imaging method of choice due to its excellent soft-tissue resolution. On T2-weighted imaging, it shows a high signal in the diverticulum due to the presence of fluid inside it. Vaginal ultrasonography is highly sensitive in diagnosing the diverticulum, but it is strongly dependent on the skills of the operator.[15]
Other diverticula
- A diverticulum of Kommerell is an outpouching (aneurysm) of the aorta where an aberrant right subclavian artery is located.[16] It is unusual nomenclature, in that focal dilatations of a blood vessel are properly referred to as aneurysms.
- Cardiac diverticulum is a very rare congenital malformation of the heart that is usually benign.[17]
Gallery
 Meckel's diverticulum
Meckel's diverticulum Large bowel (sigmoid colon) showing multiple diverticula: the diverticula appear on either side of the longitudinal muscle bundle (taenium).
Large bowel (sigmoid colon) showing multiple diverticula: the diverticula appear on either side of the longitudinal muscle bundle (taenium). Colonic diverticulum
Colonic diverticulum Diverticulum of the urinary bladder of a 59-year-old man, transverse plane
Diverticulum of the urinary bladder of a 59-year-old man, transverse plane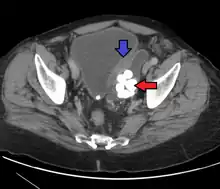 Bladder diverticula containing stones: the bladder wall is thickened due to possible transitional cell carcinoma.
Bladder diverticula containing stones: the bladder wall is thickened due to possible transitional cell carcinoma.- Bladder diverticula as seen on ultrasound with doppler[18]
- Bladder diverticula as seen on ultrasound[18]
See also
References
- ↑ "diverticulum | Definition of diverticulum in English by Lexico Dictionaries". Lexico Dictionaries | English. Archived from the original on 17 July 2019. Retrieved 17 July 2019.
- 1 2 3 Townsend, Courtney M. Jr.; Daniel Beauchamp, R.; Mark Evers, B.; Mattox, Kenneth L. (2017). Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice (20th ed.). Philadelphia, PA. ISBN 9780323299879. OCLC 921338900.
{{cite book}}: CS1 maint: location missing publisher (link) - 1 2 3 Sadler, Thomas W. (2012). Langman's Medical Embryology (12th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. ISBN 9781451113426. OCLC 732776409.
- ↑ Standring, Susan (2016). Gray's Anatomy: The Anatomical Basis of Clinical Practice (41st ed.). [Philadelphia]. ISBN 9780702052309. OCLC 920806541.
{{cite book}}: CS1 maint: location missing publisher (link) - ↑ Yam, Julie; Ahmad, Sarah A. (2019), "Esophageal Diverticula", StatPearls, StatPearls Publishing, PMID 30422453, retrieved 17 July 2019
- ↑ Barat, M.; Dohan, A.; Dautry, R.; Barral, M.; Boudiaf, M.; Hoeffel, C.; Soyer, P. (October 2017). "Mass-forming lesions of the duodenum: A pictorial review". Diagnostic and Interventional Imaging. 98 (10): 663–675. doi:10.1016/j.diii.2017.01.004. PMID 28185840.
- ↑ O'Rourke, Ashli K.; Weinberger, Paul M.; Postma, Gregory N. (May 2012). "Killian-Jamieson diverticulum". Ear, Nose, & Throat Journal. 91 (5): 196. doi:10.1177/014556131209100507. ISSN 1942-7522. PMID 22614553.
- ↑ Feuerstein, Joseph D.; Falchuk, Kenneth R. (August 2016). "Diverticulosis and Diverticulitis". Mayo Clinic Proceedings. 91 (8): 1094–1104. doi:10.1016/j.mayocp.2016.03.012. ISSN 1942-5546. PMID 27156370.
- ↑ Shah, Jamil; Patel, Kalpesh; Sunkara, Tagore; Papafragkakis, Charilaos; Shahidullah, Abul (April 2019). "Gastric Diverticulum: A Comprehensive Review". Inflammatory Intestinal Diseases. 3 (4): 161–166. doi:10.1159/000495463. ISSN 2296-9365. PMC 6501548. PMID 31111031.
- ↑ Elsayes, Khaled M.; Menias, Christine O.; Harvin, Howard J.; Francis, Isaac R. (July 2007). "Imaging manifestations of Meckel's diverticulum". AJR. American Journal of Roentgenology. 189 (1): 81–88. doi:10.2214/AJR.06.1257. ISSN 1546-3141. PMID 17579156. S2CID 45677981.
- ↑ Sagar, Jayesh; Kumar, Vikas; Shah, D. K. (October 2006). "Meckel's diverticulum: a systematic review". Journal of the Royal Society of Medicine. 99 (10): 501–505. doi:10.1177/014107680609901011. ISSN 0141-0768. PMC 1592061. PMID 17021300.
- ↑ Stunell, H; Buckley, O; Geoghegan, T; O’Brien, J; Ward, E; Torreggiani, W (2008). "Imaging of adenomyomatosis of the gall bladder". Journal of Medical Imaging and Radiation Oncology. 52 (2): 109–117. doi:10.1111/j.1440-1673.2008.01926.x. ISSN 1754-9477. PMID 18373800. S2CID 42685012.
- ↑ Chaudhery B, Newman PA (2014). "Small bowel obstruction and perforation secondary to primary enterolithiasis in a patient with jejunal diverticulosis". BMJ Case Reports. 2014: bcr2014203833. doi:10.1136/bcr-2014-203833. PMC 3962938. PMID 24626387.
- ↑ Oxford American Handbook of Urology. Albala, David M. Oxford: Oxford University Press. 2011. ISBN 9780199707720. OCLC 655896560.
{{cite book}}: CS1 maint: others (link) - ↑ Greiman, Alyssa K.; Rolef, Jennifer; Rovner, Eric S. (2 January 2019). "Urethral diverticulum: A systematic review". Arab Journal of Urology. 17 (1): 49–57. doi:10.1080/2090598X.2019.1589748. ISSN 2090-598X. PMC 6583718. PMID 31258943.
- ↑ Raymond, Steven L.; Gray, Sarah E.; Peters, Keith R.; Fatima, Javairiah (25 June 2019). "Right-sided aortic arch with aberrant left subclavian artery and Kommerell diverticulum". Journal of Vascular Surgery Cases and Innovative Techniques. 5 (3): 259–260. doi:10.1016/j.jvscit.2019.02.009. ISSN 2468-4287. PMC 6600077. PMID 31304436.
- ↑ Vazquez-Jimenez, Dr. Jaime (2003). "Cardiac diverticulum" (PDF). Orphanet Encyclopedia. Retrieved 14 January 2008.
- 1 2 "UOTW #56 - Ultrasound of the Week". Ultrasound of the Week. 21 August 2015.